Summary: SilverScript plans are standalone Medicare Part D prescription drug plans offered by Aetna for individuals with Medicare. These popular drug plans are available across the United States and have a huge network of more than 44,000 pharmacies. There are three types of SilverScript plans available. Estimated Read Time: 7 min
What is SilverScript?
Since it was founded, SilverScript has been one of the biggest providers of Medicare Part D prescription drug plans in the United States. SilverScript Insurance Company was originally founded in 2006 and sold prescription drug plans as a subsidiary under CVS Health. The CVS and Aetna merger in 2018 paved the way for SilverScript to become part of Aetna Medicare in 2021. Today, SilverScript prescription drug plans are offered through Aetna.
Aetna SilverScript plans are standalone prescription drug plans (PDPs) that you can enroll in to supplement your Original Medicare coverage. These plans help pay for generic and brand-name prescription drugs. SilverScript plans are available in all 50 states, with more than 44,000 pharmacies in their network.
SilverScript Prescription Drug Plans
Aetna offers three different SilverScript prescription drug plans with varying coverage levels and costs. Each SilverScript plan provides low copayments for generic drugs and a comprehensive drug list (formulary). All SilverScript plans have access to Aetna’s wide network of pharmacies, as well as the CVS Caremark Mail Service Pharmacy.
Though there are many similarities between SilverScript plans, there are many differences when it comes to cost and coverage. When comparing Medicare Part D plans, you should consider the following:
- How much can you afford for your monthly premium?
- What medications do you take and what quantity?
- On your current budget, what is the maximum you can afford for an annual deductible?
Monthly premiums for SilverScript plans will not only vary depending on the type of plan but will also vary by location. If you have Medicare Part B, you will need to pay your Part B premium in addition to your SilverScript plan premium. Keep that in mind when figuring out your budget.
Having a list of which medications you take and how much you take will help ensure you get the drug coverage you need. Whether or not your prescriptions are mostly generic or brand-name can also be an important consideration when comparing SilverScript plans. For example, if you take mostly generic drugs, you may be able to get a plan with sufficient coverage and a low premium.
When comparing SilverScript plan deductibles, take your medications into consideration. Plan formularies can have a significant impact on whether you end up paying your deductible. For example, a SilverScript plan may offer to cover all drugs on tier 1 and 2 of their formulary without requiring you to meet your deductible.
Things to Know About the SilverScript Formulary
When comparing SilverScript Medicare Part D drug plans online, you will want to take time to review the plan formulary. If you are already enrolled in a SilverScript plan, you should check your plan’s formulary each year, as it can change; your SilverScript formulary in 2024 may differ from the formulary in 2025.
If you are new to Medicare or haven’t reviewed a drug plan formulary before, there are a few things you should know:
SilverScript plans, like other Medicare Part D plans, have both generic and brand-name prescription drugs on their formularies. Depending on your medical needs, you may be able to reduce your out-of-pocket costs by choosing generic drugs over brand-name drugs. Speak with your doctor about your options.
SilverScript plans have five tiers on their drug formularies. The amount you pay for a drug will depend on which tier it is on.
- Tier 1: Preferred generic
- Tier 2: Generic
- Tier 3: Preferred brand
- Tier 4: Non-preferred drug
- Tier 5: Specialty
Your SilverScript plan formulary will detail any requirements or limitations for the drugs on its list, such as quantity limits. SilverScript formularies will also highlight prescription drugs that are available through a preferred mail-order pharmacy, which can be a convenient option for many individuals.
SilverScript’s Network and Preferred Pharmacies
There are many pharmacies across the nation that are within SilverScript’s network. In fact, SilverScript has over 44,000 pharmacies in its network with more than 23,000 preferred pharmacies. When looking at pharmacies within your plan’s network, you will notice that some in-network pharmacies are standard and some are preferred.
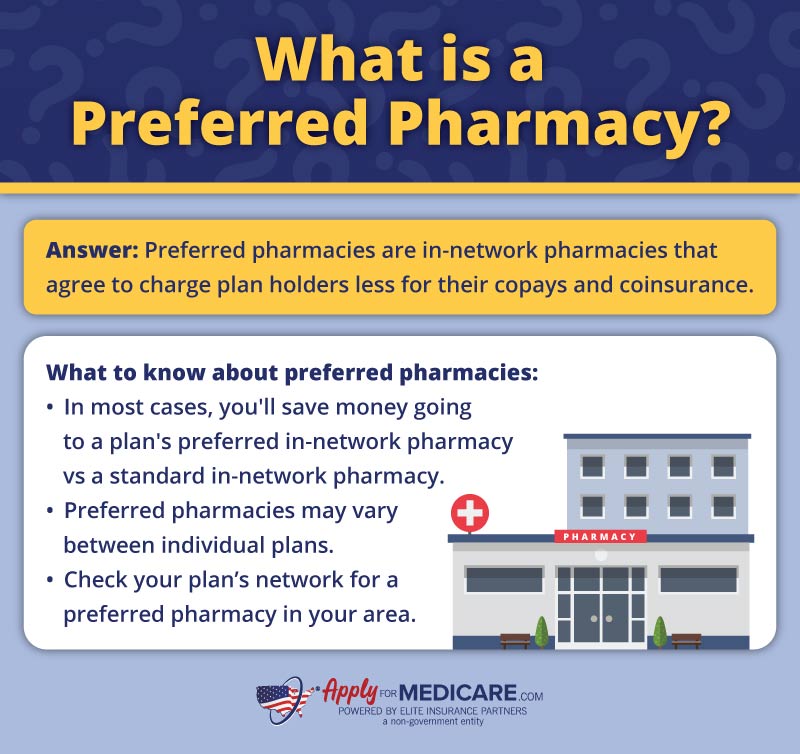
What is a preferred pharmacy? Preferred pharmacies are in-network pharmacies that agree to charge plan holders less for their copays and coinsurance. In most cases, going to your plan’s preferred in-network pharmacies will save you money when compared to going to standard in-network pharmacies.
For example, your copayment for a generic drug at a standard in-network pharmacy may be $12.00. However, that same drug may only cost you $5.00 when using a preferred in-network pharmacy.
Examples of SilverScript Preferred Pharmacies for 2025
- CVS
- Kroger
- Walmart
- Fry’s Food & Drug
- Safeway
- Publix
This is not a complete list of preferred pharmacies for SilverScript. Preferred pharmacies may vary between individual SilverScript prescription drug plans. You may live in an area that does not have any preferred pharmacies. In that case, using a standard in-network pharmacy will still save you money compared to going outside of your plan’s network.
Standard in-network pharmacies (for most plans) include Walgreens, Rite Aid, Giant, Sam’s Club, and many neighborhood pharmacies. You can find standard and preferred pharmacies in your SilverScript plan network by using Aetna’s find a pharmacy tool.
SilverScript Reviews and Customer Care Services
SilverScript is a popular option for prescription coverage for individuals enrolled in Medicare. According to KFF.org, over 6 million Americans enrolled in a stand-alone Medicare prescription drug plan through CVS Health (Aetna, SilverScript) in 2025.
Aetna provides phone support for its SilverScript PDPs 24 hours a day, seven days a week. In addition to support through customer service, Aetna also provides many online tools to help you navigate and manage your prescription drug plan.
CVS Caremark for Prescription Management
SilverScript plan holders can use CVS Caremark for prescription management and mail delivery services. Caremark makes it easy to:
- Check your drug costs and coverage
- Review your prescription history
- View and print your SilverScript plan’s Explanation of Benefits (EOB)
- Order prescription refills from the CVS Caremark Mail Service Pharmacy
A CVS Caremark app is also available to download for your smart device. The app makes it easy and convenient to manage your SilverScript plan and benefits.
CVS Caremark Mail Service Pharmacy
Individuals enrolled in a SilverScript plan can utilize the CVS Caremark Mail Service Pharmacy. Using a mail-order pharmacy is a convenient option for receiving your prescriptions. For SilverScript plan holders, you can order a 90-day supply of your prescription to be delivered to your home or location of choice. Standard shipping is free, and medications are shipped in unmarked, secure packaging to protect your privacy.
To utilize the CVS Caremark Mail Service Pharmacy, your drug must be eligible for delivery by mail (as specified on your plan’s formulary), and you must order a 90-day supply.
How To Sign Up for a SilverScript Part D Plan
Before you can sign up for a SilverScript drug plan, you must be enrolled in Medicare Part A and/or Medicare Part B. Once you have at least one part of Original Medicare, you can sign up for SilverScript during a valid enrollment period.
Like other Medicare Part D plans, you can enroll in a SilverScript plan during your initial enrollment period, during the annual enrollment period, or during a special enrollment period.
When choosing a prescription drug plan, it’s essential to review the plan terms and formulary before enrolling. Have a list of your current medications on hand so you can check to make sure they’re included in the plan’s formulary. While reviewing the different SilverScript plans, we recommend taking the time to check which in-network pharmacies are closest to you. Remember, SilverScript plans have preferred pharmacies within their network which may reduce your out-of-pocket costs.
Sources
Medicare prescription drug coverage, Aetna. Accessed October 2023
https://www.aetnamedicare.com/en/faq/part-d-prescription-drug-coverage.html
Key Facts About Medicare Part D Enrollment and Costs in 2023, KFF.org. Accessed October 2023
Aetna Medicare RX Delivery, Aetna. Accessed October 2023
https://www.aetnamedicare.com/sites/mailorderpharmacy.html
United States v. CVS and Aetna Questions and Answers for the General Public, U.S. Department of Justice. Accessed October 2023
https://www.justice.gov/opa/press-release/file/1099806/download

